Objectives of cleaning and disinfection
Cleaning is intended to remove matters (e.g., patient secretion and inorganic material (e.g., salts) from surfaces of reusable medical devices (RMD)
Disinfection, is intended to reduce the microbial load
Cleaning and/or disinfection takes place in preparation for sterilization or with disinfection as a final step before use of the RMD.
- Before sterilization, the primary objective is cleaning i.e. the withdrawal of matter which would interfere with the sterilizing agent and generate endotoxin or pyrogen risks. Disinfection improves the preparation of RMD for sterilization and is required or recommended in some countries as an occupational health and safety measure for operators in charge of packaging .
- As the last step before use of the RMD, the objective of cleaning & disinfection is to render the RMD safe for the patient according to Spaulding classification principles.

In the present guide cleaning&disinfection is preferred to decontaminationPrinciples of cleaning
Cleaning consists of washing followed by rinsing
- Washing is the removal of soils from surfaces of the RMD by water containing a cleaning agent.
- Rinsing evacuates the soils detached by washing as well as detergent residues which would chemically interact with disinfection or sterilization agents.
Main categories or detergent are : neutral, with or without enzymes, mild alkaline with or without enzymes, alkaline
| Most detergent formulations include a surfactant (to reduce the surface tension of water thus easing the wetting of surface and breaking up of soils). Other components of detergents are buffers to improve the compatibility with RMD material and Softeners to reduce the potential negative effect of hard water (spotting and deposit on surface). Neutralizers may be applied after some alkaline cleaners. Cleaning agent comply to applicable local detergent regulation See disinfection paragraph for formulation used for combined cleaning and disinfection They is no international standard for detergent but methods and thresholds are becoming available to evaluate cleaning efficacy. |
Cleaning is performed according to instructions for use of RMD manufacturer and cleaning agent manufacturer
| The conditions for efficient washing are illustrated by the Sinner circle1. Mechanical action by manual brushing, flushing, swabbing or wiping, automated spraying or flushing, cavitation (in ultrasonic cleaner).2. Chemical action of cleaning agents which decompose protein, fats, ease the removal or soil from surfaces3. Contact time of all RMD surfaces with the cleaning/water solution4. Temperature of the cleaning solution.Concentration, exposure time or temperature above those specified by IFU may present risk for operators and damage on RMD and do not mean higher cleaning efficacy. Progress of minimally invasive surgery often means complex, narrow geometries (lumen, cavities, hinges) more susceptlble to retain soil, delicate and hidden to visual control. If specified by RMD manufacturer instruction for use (IFU), multicomponent RMD are disassembled prior to cleaning. |
Consistency of cleaning (i.e. rigourous application of cleaning procedure after each use of the RMD) is key to avoid the progressive formation of biofilm or build-up of mineral deposit in narrow spaces or cavities
| Once installed, biofilms (for instance biofilms of Pseudomonas aeruginosa) protect the germs from disinfection agent. Biofilms are likely to grow and become more difficult to withdraw even if next cleaning is well performed.Build-up of mineral deposit (for instance scale) ease the anchorage of germs and biofilms, damage instruments and impair their functionalityScratches or rust facilitate the anchorage of soils and biofilms. Damaged or rusted RMD are sent for maintenance or discarded. |
Principles of disinfection Disinfection is chemical or thermal
- Chemical disinfection with a disinfection or cleaning & disinfectant formulation is followed by rinsing, drying and when recommanded by RMD IFU, by lubrication Chemical disinfection is mainly used for thermosensitive RMD.
| Rinsing with adequate water quality removes chemical agent residues. Rinsing after disinfection is called final rinsing to differentiate it from intermediary rinsing which takes place after cleaning.Drying with adequate air quality removes residual humidity which favors recontamination and impairs sterilization. In some countries, alcohol rinsing is used to accelerate drying (in particular for GI endoscope reprocessing). This practice is not allowed in other countries (for instance Europe) due to fixative properties of alcohol. |
RMD is immersed in a bath (manual process), exposed to spray (automated process) or wiped (only when immersion or spray are not allowed by RMD manufacturer IFU).
Chemical disinfection is achieved when all RMD surfaces have been exposed to the disinfecting formulation at concentration, temperature and for the contact time specified by the disinfectant manufacturer instructions for use (IFU).
Disinfection is characterized by the achievement of a specified log10 reduction on of representative test microorganisms (Unlike sterilization which targets eradication of all microorganisms)
| Categories of microorganisms are listed below in order of usual growing order of resistance to disinfectant (examples of microorganisms frequently used for tests appear in brackets)Vegetative bacteria – gram negative and gram positive (for examples, Staphylococcus aureus, Pseudomonas aeruginosa)Fungi/yeast (Aspergillus niger, Candida albicans)Virus : enveloped (lipid or medium size) viruses such as HIV, herpes, hepatitis are less resistant than bacteria while non-enveloped (nonlipid or small viruses such as polio).Mycobacteria (M. tuberculosis, M. terrae, M. avium)Spores (Bacillus. atropheus, B. subtilis, B. cereus, Clostridium sporogenes) Prions are more resistant than all the above.Each claim (bactericidal, fungicidal, virucidal, mycobactericidal, sporicidal) is validated separately. For instance, a successful sprocidal test, does not yield a claim with germs of lower resistance.Tests microrganisms are protected by artificial soil simulating the level of organic matter which may be found on RMD. Disinfectant used after cleaning are tested in clean conditions. Disinfectant used for combined cleaning and disinfection are tested in dirty conditions.There are no unique ISO international standards for evaluation of disinfecting activities. Tests protocols are hence subject to regional variances. For instance, it is generally agreed that carrier tests are the more representative for RMD but despite harmonization effort under the Organisation for Economic Co-operation and Development (OECD) test protocols (methods and log reduction objectives) differ (AOAC or ASTM in USA, phase 2.2 EN test in Europe). Carrier test are methods in which microorganisms are inoculated and dried on an inanimate surface before being immersed in the disinfection solution. |
Chemical disinfectants formulations are aldehydes (Glutaraldehyde, Ortho-phthalaldehyde-OPA) and peracetic acid. Detergent-disinfectants use chemical with dual properties or mixtures of detergent and disinfectant
| Aldehydes have good compability with RMD. Room ventilation is required for glutaraldehyde due to irritancy and potential toxicity.OPA is better tolerated. Aldehyde are fixative of protein and must be only be used after thorough cleaning. Formaldehyde which also belongs to the aldehyde disinfection family is a carcinogen and not anymore used.Peracetic acid has a broad spectrum of activity and good efficacy on spores but is less stable and more corrosive than aldehydes. Unlike aldehydes it produces no toxic waste.Other formulations based on hydrogen peroxide, chlorine based, chlorine dioxide (ClO2) may be found. Compatibility with materials of RMD must be checked. Alcohol is not an effective disinfectant for RMD (it does not penetrate well into organic material and is not sporicidal) .Combined cleaning and disinfecting chemical formulations are mixtures of quarternary ammonium, biguanide, guanidine, alkylamine, enzymatique, alkaline. Aldehyde based cleaner-disinfectant are avoided due to their fixative properties. |
Choice of disinfectant is made in partnership with infection control. Disinfectant must be effective on the type and quantity of mircroorganisms which may be present on the RMD.
| For instance, nature as well as amount of microorganisms present on RMD are not be the same for gastroscopes and bronchoscopes.Additional precautions may be required in special circumstances (for instance a C. Difficile breakout).Fragile or immunodeficient patients may require additional precautions.Choice of formulation might be influenced by local habits, recommendations or regulations, for instance in regards to fixative properties or for waste management considerations. |
- Thermal disinfection is performed in automated washer-disinfectors (WD) with hot water at specified temperature Thermal disinfection is commonly used for surgical instruments intended for steam sterilization. Lubrication is applied as recommended by RMD manufacturer IFU.
Reusable containers and other heat and moisture compatible items are also thermally disinfected.In thermal WD Disinfection and rinsing are combined. Thermal disinfection provides good drying. Thermal disinfection is also efficient for self-disinfection the washer-disinfector.
Some manufacturers may however offer or recommend periodic self-disinfection cycles
Thermal disinfection, is achieved when all RMD surfaces have been exposed to hot water at a defined temperature for a minimum contact time.
Thermal disinfection is efficient to eliminate most microorganisms. Spores show higher resistance. Thermal disinfection can be characterized by the A0 concept
| The improvement of lethality with hot water temperature can be predicted. For instance, for heat resistant microorganisms, 10 minutes at 80°C has the same lethality effect as 1 minute at 90°C or 100 minutes at 70°C. By convention the time (expressed in second) to obtain a given log reduction at 80°C serves as a reference and called A0 for heat resistance microorganism. In the above example A0 equals 600 s (10 minutes at 80°C). Higher A0 means longer exposure time at 80°C or shorter times at higher temperature according to A0 equation. A0 = Σ10[(T-80)/z] x êtSee annex B of international standard ISO 15883-1 for more explanation. Local regulation, recommendation or habits define the A0 thresholds according to the level of contamination of the RMD and intended use.A0 of 60 s is commonly recognized as the minimum to be targeted for low risk items according to Spaulding classification principles. 600 s is the minimum for other items. Automated WD for surgical instrument complying to ISO 15883-2 must have one cycle with an A0 value above 3000 (e.g. a theoritical value of 50 minutes at 80°C or practically 5 minutes at 90 °C or 2 min and 30 s at 93 °C).A0 values of 3000 or above are recommended in some countries. Others consider 600 s as sufficient for most items (considering that thermal disinfection always takes place after cleaning and that residual spores (if any) will be eradicated by sterilization Some national regulation (for instance FDA in USA) may not recognize the A0 concept and have other ways to specify the minimum level of disinfecting efficacy to be achieved by thermal washer for RMD on a defined thermophilic mycobacterium species. |
After disinfection, RMD may still carry some microorganisms, residual humidity and are not protected by packaging. Precaution must be taken to limit environmental and handling contamination.
Maximum storage time after disinfection are usually defined by local recommandation or regulation.Choice of cleaning & disinfection process
The 4 main categories of cleaning and/or disinfection processes are
- Manual cleaning & Disinfection. RMD are immersed and manually processed in cleaning and then disinfection baths or in combined cleaning&disinfection solutions. When immersion is not allowed by RMD manufacturer IFU, RMD is wiped.
- Automated washer disinfector. Disinfection if thermal or chemical
- Ultrasonic cleaning, when approved by RMD manufacturer IFU
- Automated Endoscope Reprocessors (AER) for thermosensitive flexible endoscopes
Choice of cleaning & disinfection process, cleaning, disinfection and lubrication agents take into account instruction for use (IFU) of RDM, detergent and cleaning equipment manufacturers
| RMD manufacturer IFU specify the compatible cleaning and disinfection methods. Compatibility means that evidence are available that the RMD can be efficicently cleaned and disinfected and remains functional and safe for use. If appropriate, the manufacturer of the reusable medical device (RMD) indicates a maximum number of reprocessings allowed.WD and ultrasonic cleaners manufacturersrecommend the type of detergent and disinfectant approved and tested for use with their technology as well as dosage. Manufacturer of the equipment checks efficacy of cleaning and disinfection agent approved for use in the more unfavorable conditions (for instance lowest value of the temperature range)IFU of cleaning and disinfecting agent Manufacturers – indicates if the chemistry is intended for manual, automated or ultrasonic cleaning – gives dosage, contact time, T°C, water quality for each usage – specifies precaution for use, waste management, time during which an open detergent or disinfectant bottle can be used. Labeling carries the expiry date. |
When allowed by RMD manufacturer IFU,automated cleaning and disinfection processes (WD and AER) are preferred to manual.
Washer-disinfector (WD) and automated endoscope reprocessors(AER) are more reproducible (less human dependant) and safer for operators (reduction of exposure to chemicals, aerosols, handling risk).
Automatic recording allows reliable documentation.
For cleaning and disinfection of RMD in preparation for steam sterilization International standards express a preference for thermal disinfection

ISO 15883-12 says: Thermal disinfection processes are more easily controlled and avoid the hazards to staff, patients and the environment that can occur through the use of chemical disinfectants. “Thermal disinfection is efficient to eliminate most microorganisms (except spores) and provide good rinsing and drying”.
Manual or ultrasonic pre-cleaning may be required before automated cleaning and disinfection of complex and/or heavily soiled RMD
| Place of ultrasonic cleaning in national or regional guidelines depends on regional habits, guidelines or regulations. In some countries ultrasonic cleaning is only used for pre-cleaning of heavily soiled or complex RMD before automatic cleaning. In other countries, ultrasonic cleaning may plays a larger role. |
Manual wiping is used when immersion in bath is not allowed by RMD manufacturer IFU

International standard ISO 176648says :
At least one validated automated cleaning method (which may include a validated manual pre-cleaning method) shall be specified unless the medical device cannot withstand any such process, in which case a statement shall be provided which alerts the user to this issue……. A validated method of manual cleaning shall be specified if automated cleaning is not possible.
if the medical device is intended to be disinfected, at least one validated automated disinfection method shall be specified unless the medical device cannot withstand any such process, in which case a statement shall be provided which alerts the user to this issue…… If the medical device is intended to be disinfected a validated method of manual disinfection shall be specified if automated disinfection is not possibleImplementation of manual cleaning & disinfection process
Manual Cleaning & disinfection processes are prepared and implemented according to written standard operating procedure (SOP).
Preparation of Cleaning and disinfection baths is according to the IFU of the cleaning agent manufacturer. Water quality used for each step is as recommended per IFU (water hardness, pH, temperature).
Brushes, single-use cloth and other cleaning accessories are as recommended by RMD Manufacturers instruction for use (IFU) or equivalent to them (usually soft nylon bristle brushes). Unless clearly specified in the RMD metallic brushes are not used. Type, size (diameter and length), bristle type and material of brushes used to clean lumen are those indicated in RMD manufacturer IFU. They should be the same diameter as the lumen to ensure all internal surfaces can be reached and long enough to exit the distal end of the instrument. RMD manufacturers may have special recommendation for optics surfaces.
If not single use, brushes are daily cleaned, disinfected (preferably thermal) and dried. Brushes are checked after each use and replaced when damaged.
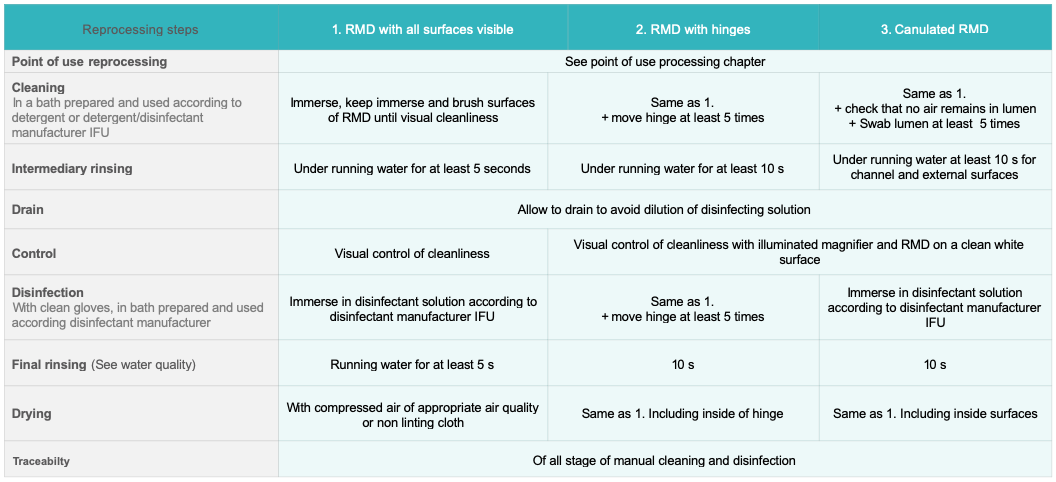
Steps are as follows:
- The RMD is completely immersed in the cleaning bath. Articulated RMD are open to minimize obscured surface area. Bubbles trapped in cavities and channels are eliminated. Some manufacturers may recommend flushing through at a specified pressure for a defined time. RMD remains immersed during cleaning. Cleaning operations are performed in a manner that limits production of aerosols or dispersion of potential contaminated chemicals or water.
- Gross soil is removed. Accessible surfaces are cleaned with appropriate tools until visibly cleaned. RMD with articulations are moved (open and close at least 5 times). Channels are swabbed. Swabbing is always performed in the same direction from the less soiled to the most soiled end (at least 5 times). Other hard to access area are flushed with syringe, water gun or hand pump
- RMD is rinsed under running water (at least for 10 s for all external surfaces). Articulations are moved. Channels are flushed for at least 10 s. RMD is allowed to drain to avoid dilution of disinfection solution. Rinsing removes visible or non visible soil as well as residual detergent which might react with disinfectant.
- Absence of soil is visually checked. RMD and canulated device are placed on a white clean surface (for instance white crepe papier) and observed under illuminated magnifier
- RMD is immersed in disinfection bath. Articulations are moved at least 5 times. It must be checked that internal lumen and cavities and completely immersed and in contact with solution.
- RMD is rinsed with appropriate water quality: 10 s at least for all external surface and 10 s flush for each channel.
- RMD is dried with adequate compressed air quality. If compressed air is not available or not recommended by the manufacturer RMD is air or hand dried with a disposable clean, non-linting cloth.
If manual cleaning and disinfection is performed with a cleaning-disinfecting agent steps 2 and 3 are skipped and visual control is performed after 6.
The disinfection bath is preferably single use. If not, the disinfectant manufacturer specify the maximum number of reuse and provide recommandations and means to control that the concentration of disinfection agent is above minimum levels required for efficacy.
SOP details the steps and, for instance, provide quantitative and qualitative indication for manual operation, number of time a channel should be brushed or flushed and criteria, accessories to be used
It might be convenient to organize Manual cleaning and disinfection SOP according to RMD configuration.
For RMD or parts of RMD which cannot be immersed (for instance some motors, batteries) are wiped and rinsed with disposable cloth soaked with detergent and/or disinfectant agents. Consistency of manual wiping is difficult to obtain. Manual wiping is used when non other cleaning and disinfection methods are applicable. Manual wiping is carried according to RMD manufacturer IFU.
Manual wiping steps are as follows:
- Wipe with a disposable, clean, non-linting cloth and detergent until all cleaning agent residue is visually removed. Check that moisture does not penetrate into critical parts of the device (for instance power or electronic connections)
- Rinse the RMD by wiping surface thoroughly with a damp, disposable, clean, non-linting cloth with objective to withdraw disinfection residues.
- RMD is visually controlled if needed with an illuminated magnifier
- Dry with medical-grade compressed air. If compressed air is not available or not recommended by the manufacturer of the RMD, air dry or hand-dry using a disposable clean, non-linting cloth. Disposable cloth are discarded
If wiping is performed with a cleaning.disinfecting agent (non-critcial RMD only) steps 2 and 3 are eluded.Implementation of ultrasonic cleaning process
Ultrasonic cleaners use cavitation to detach soils from RMD.
| Ultrasound generators produce acoustic waves (waves frequency generally ranges between 35 and 45 kHz). Acoustic waves create bubbles which implode as they become larger and unstable. Implosion creates a vacuum in the solution (cavitation) that mechanically draws debris from the surface of the RMD.Ultrasonic cleaners encompass a wide range of technologies from the basic ultrasonic cleaning equipment with the user performing all the function of filling, rinsing, draining to automated equipment. Ultrasonic cleaners could be categorized as follows : (basic) ultrasonic cleaners, ultrasonic irrigators or irrigator-washer or irrigator washer-disinfector. |
Efficacy of cavitation is improved by adapted cleaning agent.
Ultrasonic cleaner are often used for pre-cleaning (prior to Washer-disinfector) of complex RMD.
Ultrasonic cleaners are well adapted for stainless steel devices with reamers (rasps) , lumen, sleeves or complex shapes difficult to access.
Ultrasonic cleaning is used only if not contraindicated by RMD IFU
| Ultrasonic cleaning is not recommended for RMD with :Some types of adhesivesMixing different metals (for instance scissors with screw, needle holder, clamps with jaws in tungsten carbide, chrome or nickel steel)Optics (because of the risk for adhesives and seals)Power toolsOther active items such as phacoemulsification or dental handpieces |
Ultrasonic cleaning processes are prepared and implemented according to written standard operating procedure (SOP).adapted to ultrasonic cleaner features.
Detergent must be suitable for ultrasonic cleaner.
Before immersion in ultrasonic bath RMD gross soil is removed.
Principles for bath preparation, loading and unloading are as follows
- Follow instructions of ultrasonic cleaner and detergent manufacturers for dosing and temperature of bath. Water temperature is between 27 °C (80 F) and 43 °C (109 F) and never above 60 °C (140 F) because most proteins denaturate above that temperature. For ultrasonic systems without thermoregulation room temperature might be preferable as energy delivered by ultrasonics wave will increase the temperature of the bath.
- The bath is degassed at each filling. This is done by filling the unit, closing the lid and running a cycle for 5 to 10 minutes
- RDM are placed in a tray (never directly on tank end) widely opened, not superposed to avoid shadow. When applicable, connect lumen devices to flushing ports. If other specific positioning accessories and features are used, refer to manufacturer IFU.
- The cavitation process may create aerosols, the ultrasonic bath should hence have a lid that must remain closed during the cleaning process.
- Process timeis as recommended per manufacturer (usually between 5 and 10 minutes)
- If rinsing is not performed by the ultrasonic cleaner, the RMD is rinsed and dried manually
The bath is preferably changed after each use (i.e. after reprocessing cycle). Ultrasonic cleaning equipment is cleaned every day that it is used and according to manufacturer IFU. Local recommendations specify that it has to be refilled after each use or daily and each time the bath is visibly soiled.

National regulation or recommandation may forbid the use of ultrasonic cleaners if a prion riskhas been identifiedImplementation of washer-disinfector processes
Washer-Disinfectors spray or flush pressurized water mixed with a detergent on surfaces of RMD and lumen. The cleaning stage is followed by a thermal or chemical disinfection.
Various types of WD and applicable international standards are as follows :
- Washer-disinfectors with thermal or chemical disinfection stage for surgical instruments. There are available in different construction, e.g. single chamber (load-through or single door) or multichamber version.
- Thermolabile endoscope washer-disinfector
- Cart-washer for the cleaning of carts, reusable containers, surgical basins and other non-invasive , non-critical medical devices.
- Multichamber WD
- Washer-disinfector for dental handpieces and turbines

International Standard ISO 15883 family includes general requirements ISO 15883-1 and specific parts dedicated to each type of WD
- WD for instruments comply with ISO 15883-1 and -22,3
- WD for thermolabile flexible endoscope comply with ISO 15883-1 and -41,5
- Cart washer comply with ISO 15883-1 and -6 (thermal disinfection) or -7 (chemical disinfection)1,6,7
There is currently no ISO standard for dental handpieces and turbines

Compliance to ISO 15883-12 and subsequent parties2,3,4,5,6,7 may be required (for instance in Western Europe)
WD processes are prepared and imlplemented according to written standard operating procedure (SOP).
Heavily soiled and/or complex RMD may require manual or ultrasonic precleaning
As per RMD manufacturer IFU, RMD is disassembled, cap, gaskets, all disposable items are removed. Hinged surgical instrument with handles (scissors, clamp, and forceps) are opened (generally at 90°) according to manufacturer IFU
The SOP describes the load configuration(i.e. the type of RMD which can be reprocessed together in a given cycle).
RMD are placed in a tray or positioned on suitable modules and/or connected to irrigation ports (for lumen devices).
| If needed hold-down screens or retaining systems prevent dislodging of RMD during the cycle.Fragile or small devices are protected (installed in trays with lid and/or blocking accessories).Heavy or large items are preferably placed on lower-levelsHollow items are turned downwards for water evacuationRacks should never be overloaded. All RMD surfaces must be exposed to water spray (no shadowed surface).Specialized racks and loading equipment are required for RMD with complex geometries and lumen. Racks are for instance available for laparoscopic surgery, dentistry, robotic surgery.Minimally Invasive Surgery (MIS) instruments with lumen are connected to adaptors. Adaptors are carefully chosen for proper flushing pressure and flow. Clear procedures are key to optimize the layout, avoid connection mistakes or accidental disconnection during cycles. In case of especially narrow lumina a filter is required to prevent particles from entering the lumen. |
Before cycle launch it is checked that spraying arms are unobstructed.
All phases of WD cycles are automatically run, controlled and recorded. WD cycles usually start with a pre-washing phase (included in the automated cycle) to wet the RDM but does not replace ultrasonic or manual pre-washing.
- Pre-washing wets the RMD (without detergent) to ease soil removal.
- Washing is at temperature is at temperature specified by detergent manufacturer (usually around between 45 °C. Mechanical action is by spray, circulation or irrigation). cleaning solution is single use
- Intermediary rinsing may include a neutralization stage (for some cleaning agent formulations)
- Thermal (preferred if applicable) or chemical disinfection is adapted to contaminants and log reduction targets. In chemical WD, if the disinfection is not single use, the maximum number of reuse specified by the disinfectant manufacture is respected. Recommendations and means are provided by the manufacturer to control that the concentration of disinfection agent is above minimum levels required for efficacy.
- Final Rinsing. In thermal WD thermal disinfection also serves as a rinsing phase.
- Drying is obtained by circulation of hot air (of appropriate air quality)
Implementation of automated endoscope reprocessor (AER) processes
AER are used for gastro-intestinal (GI) scopes (GI) and some other semi-critical single lumen flexible endoscopes. AERspray or flush pressurized water mixed with a detergent and then a disinfectant on surfaces and lumens of the endoscopes. All phases are automatically run, controlled and recorded.
AER processes are prepared and imlplemented according to written standard operating procedure (SOP).
In chemical WDincluding AER – cleaning solution is single use, disinfection solution is preferably single use. If the disinfection solution is reusable, the user respect the maximum number of reuse specified by the disinfectant manufacturer. Recommendations and means are provided by the manufacturer to control that the concentration of disinfection agent is above minimum levels required for efficacy.Cleaning & disinfection and quality management
Written cleaning & disinfection standard operating procedures (SOP) are prepared in accordance with quality management principles. Each step of the cleaning& disinfection process is an improvement to the former steps and does not impair the efficacy of the following stages
| For instance, final rinsing and drying are performed with adapted Water quality and Air quality to avoid recontamination of the disinfected RMD. Lubricant must be compatible with the RMD and with the sterilization process. Incompatible lubricants can inhibit sterilization, create harmful by-products, and damage the device. |
User supervises or perform process validation and in particular controls that
- Installation of cleaning and disinfection workstation or equipment is conform to manufacturer recommendations
- Documentation (for instance, IFU, test and calibration certificates) are available
- Standard Operating Procedures (SOP) are up to date
| Written standard operating procedures (SOP) are available for each RMD or group of RMD requiring similar cleaning and disinfection process. For newly purchased RMD, a new SOP is defined if an existing one cannot be used.When possible SOP provide quantitative and qualitative criteria for manual operations (for instance brush until no soil is visible, number of time a lumen should be swabbed etc..) |
- Systematic and periodic routine controls are in place (see below)
| For all cleaning & disinfection process, RMD are visually controlled for cleanliness. If soils are visible RMD are cleaned again. For washer disinfector (WD) and automatic endoscope reprocessors (AER) processes aiming compliance to international standard ISO 15883-1, cleaning efficacy is controlled at periodicities and according to methods described in ISO 15883-1 and 15883-55. For WD and AER not aiming compliance to ISO 15883 validation framework proposed by ISO 15883 and 15883-5 methods may be used Microbiological and chemical quality of incoming and final rinsing water quality are controlled according to local regulation and meet specifications of equipment, detergent and disinfectant manufacturer IFU. Periodical Microbiological controls of RMD may be required by local regulations (for instance annual control of flexible endoscopes in some countries). |
- Occupational health & safety considerations (in particular exposure to liquid and vaporized chemicals, aerosols and injuries by potentially contaminated RMD)
- Reprocessing fluids are discarded according to local waste management rules.
- Training (including training on occupational health & safetymeasures) are up to date, executed and training certificates are available.
- Maintenance plans are in place for washer-disinfector, ultrasonic cleaners and dosing pumps.
- Traceability is operational

WFHSS key recommendations for cleaning & disinfection
- Cleaning & disinfection process complies to instructions for reprocessing of RMD manufacturer. It is implemented according to IFU of RMD, detergent, disinfectant and reprocessing equipements manufacturers
- Thorough and consistent Cleaning is essential for efficient disinfection and sterilization. Progress of minimally invasive surgery often means complex, narrow geometries, difficult to access and hidden to visual control. Inconsistent cleaning allows the progressive development of biofilms or mineral deposits.
- Objective of disinfection depends on intended use of RMD
- When done in preparation for sterilization, disinfection improves the preparation of RMD for sterilization. It may be required or recommended in some countries as an occupational health and safety measure.
- When disinfection is the last step before use of the RMD on patient targeted efficacy is defined, with infection control, according to Spaulding classification principles .
- Automated cleaning and disinfection in WD or AER is preferred to manual
- Ultrasonic or manual precleaning may be needed for complex or heavily soiled RMD. Ultrasonic reprocessing must be allowed by RMD manufacturer IFU.
- Thermal WD are preferred for heat and moisture resistant RMD.
- WD and AER are preferably compliant to international standardsprocesses complying to international standards1,2,3,4,5,6,7
- Non automated cleaning & disinfection is performed with care and consistency. When allowed by RMD manufacturer IFU, ultrasonic cleaning is efficient for devices with complex geometries. Wiping is used only when RMD manufacturer IFU do not allow immersion. Combined manual cleaning and disinfection with a cleaning&disinfecting formulation may be used on low risk items according to Spaulding classification principles or, if permitted by local regulation, in preparation for sterilization.
- Manual and automated cleaning and disinfection processes are implemented according to quality management principles. Standard operating procedures (SOP) are up to date and describe systematic or periodic (visual controls of cleanliness and dryness are systematic). Process validation concerns both automated and manual processes. International standards1,5 Operators training is regularly updated and controlled. Appropriate occupational health and safety measures and traceability are in place.