For the purpose of this guide a Reusable Medical Device (RMD) means:
- An item that is not intended by its manufacturer for single-use.
- A medical device designated or intended by the manufacturer as suitable for reprocessing.
![]() Reprocessing of single use medical devices is outside the scope of these guidelines
Reprocessing of single use medical devices is outside the scope of these guidelines
RMD’s may be :
- Medical or surgical items in contact with skin, mucous, or are inserted into the human body (e.g., surgical instruments, flexible endoscopes, dental instrumentation).
- Diagnosis, monitoring, treatment equipment components in contact with a patient.
- Items used for conveying body fluids, tissues or preparation for subsequent use in humans (e.g., hemodialysis).
![]() Medical device regulations vary between regions. Some items may not be registered as medical device in some regions.
Medical device regulations vary between regions. Some items may not be registered as medical device in some regions.
Reprocessing means all operations performed on a used RMD to allow its safe reuse
![]() The European Medical Device Regulation defines reprocessing as a:
The European Medical Device Regulation defines reprocessing as a:
“process carried out on a used device in order to allow its safe reuse including cleaning, disinfection, sterilization and related procedures, as well as testing and restoring the technical and functional safety of the used device”.
The US food and drug administration (FDA) defines reprocessing as a:
“validated processes used to render a medical device, which has been previously used or contaminated, fit for a subsequent single use. These processes are designed to remove soil and contaminants by cleaning and to inactivate microorganisms by disinfection or sterilization. Reprocessing of reusable devices encompasses appropriate steps that begin in close proximity to the point of use of the device and, in general, involves the following three steps in sequence: point-of-use processing…., thorough cleaning….. Disinfection or sterilization……”
Reprocessing may be performed by a health care facility or shared with an external organization under an outsourcing contract.
Reprocessing applies to all RMD’s that were removed from packaging, even if they were not used.
Reprocessing may also be undertaken on:
- A loaned or deposited RMD,
- An RMD returned from repair,
- A new RMD delivered non-sterile. Specific reprocessing may be recommended by RMD manufacturer to eliminate manufacturing residuals from a new device and/or to sterilize the device before first use.
An RMD returned for maintenance must be cleaned and disinfected for the safety of maintenance staff (a reprocessing certificate is provided)
Instruments and items for patient care were categorized by E.H. Spaulding in the late 1960’s according to the risk for infection involved in their use.
- Critical: An item that contacts sterile tissue or the vascular system. A critical RMD presents a high risk for infection if it is contaminated by any microorganism. Thus, an object that enters in sterile tissue or in the vascular system must be sterile. Any microbial contamination could transmit disease. Surgical instruments, surgical implants, endoscopes or ultrasound probes (such as choledochoscopes) used in sterile body cavities are examples of critical RMD’s.
- Semi‐critical: An item that contacts mucous membranes or non‐intact skin. Mucous might be an efficient barrier against small quantity of common bacterial spores. However, other organisms are at risk, such as bacteria, mycobacteria, and viruses. Examples of semi-critical items are respiratory therapy and anesthesia equipment, and some flexible endoscopes.
- Non‐critical: An item that contacts intact skin but not mucous membranes. Intact skin acts as an effective barrier to most microorganisms. Examples of noncritical patient-care items are bedpans and blood pressure cuffs. Non-critical environmental surfaces include bed rails, some food utensils, bedside tables, patient furniture, and floors. In some regions keyboards and consoles forming part of imaging systems may also be classed as medical devices and these will also be non-critical.
The core principles of the Spaulding classification remains valid, however, changes have occurred over time. For example:
Minimally invasive surgery increased the average complexity of RMD. Cleaning of lumen and sophisticated devices can be difficult. Heavily soiled and contaminated flexible duodenoscopes are a good illustration where the complexity of cleaning increases the risk and sterilization may be advocated to support effective cleaning.
- Choice of sterilization and disinfection methods has increased, is more difficult, and subject to local interpretations.
Heat sensitive RMD's require a range of cycles adapted to their material and geometrical specificities. Some heat compatible, minimally invasive surgery instruments are subject to accelerated aging (e.g., laparoscopy devices). Some countries offer the flexibility to use low temperature sterilization; other countries do not. More recently, overlaps have appeared between critical and semi-critical categories. For example, an endoscope used for upper gastrointestinal tract investigation with sterile biopsy forceps. The 3 levels of disinfection defined below are not used by all guidelines.
Some countries have additional criteria for high level disinfection. For instance, the US FDA definition is: sterilant used for a shorter contact time to achieve a 6-log10 kill of an appropriate Mycobacteriumspecies. In other countries there is no efficacy threshold between intermediate and high-level disinfection and the sterilant concept is not used. National or regional regulations should be consulted with respect to use of the above categories of disinfection. |
- Prion, outbreak and patient susceptibility (e.g., immunocompromised patients) have highlighted the need for communication between care units and infection control.
- Regulators and international standards have increased the pressure on medical device manufacturers for improved, validated instructions for reprocessing. s
| International standards ISO 17664-1 describes the information to be provided by RMD manufacturer for reprocessing of critical and semi-critical medical devices. RMD manufacturers' guidance are supported by risk analysis and tests, as needed. RMD manufacturers check that the recommended reprocessing methods are available in countries where an RMD is marketed. |
- Occupational health and safety and environmental considerations became key factors. For example, automated cleaning methods are preferred as they are more consistent and safer for operators. Waste management rules are applied.
Prion is a small proteinaceous infectious unit that appears in a variety of human and animal neurodegenerative diseases, including Creutzfeldt-Jakob disease (CJd), bovine spongiform encephalopathy (BSE, also known as the mad cow disease), and scrapie.
Prion diseases have always existed but usually very rare. Prion proteins derive from a normal body protein that becomes irreversibly mis-folded. Prion proteins proliferates primarily in the central nervous system (CNS).
In the 1980’s beef became infected by BSE in some Western European countries. A variant of Creutzfeld-Jakob disease spread among human who had consumed infected beef.
Prions are highly resistant to disinfection and sterilization. Their resistance can be increased by fixative agents.
Anti-prion regulations or guidelines were hence implemented by some countries to deal with the removal or inactivation of prion proteins from RMD’s. Such regulations or guidelines are country specific. The following paragraphs provide high level information on prion recommendations (when such national or regional recommendations or rules exist).
Strategy is commonly based on patient screening and specific attention to CNS surgeries (brain, spinal cord or posterior of the eye).
Example of measures for at risk patient or surgeries are :
- When possible, prefer single use surgery devices.
- Extended hold period of an RMD until the absence of risk can be confirmed.
- Processes which experimentally showed an ability to inactivate prion (i.e., destruction of the protein and not only elimination).
| Evaluation of prion inactivation is based on complex in vivo experiments. Example of processes which show efficient are sodium hypochlorite, sodium hydroxde, high pH alkaline detergent, some low temperature sterilization cycles, combination of cleaners and low temperature cycles. Efficacy is obtained in accurately defined conditions (i.e., concentration, temperature and exposure times, etc.) and are only valid for these specific conditions. Steam cycles at 134°C 18 minutes have a high efficacy. (although inactivation is not complete) |
Prion regulation or guidelines insist on precaution to avoid drying of soils on RMD’s and include warnings on risks linked to the use of fixative processes
| Some sterilizing, cleaning and disinfecting formulations are known to reinforce the fixation of proteins, including prion, on RMD surfaces. For instance, dry heat, ethylene oxide, aldehyde based sterilizing and disinfecting agent such formaldehyde or glutaraldehyde or alcohol. Countries with prion regulation may forbid or discourage the use of fixative formulation or require a thorough cleaning with a non-fixative process before implementation of a potentially fixative formulation. |
In addition some regions may set their own standards for residual protein levels on RMD and apply additional precautions for RMD used in particular procedures such as those relating to the brain, spinal cord or posterior of the eye
As prion Management is country specific Management of prion risk is management by national regulation
Medical Device Vigilance Systems are used to improve patient safety, provide for the protection of health and safety of healthcare professionals, and other users by reducing the likelihood of reoccurrence of incidents related to the use of a RMD.
Countries have regulations in place to collect and analyse incidents report.
Some risks may be related to reprocessing. Reprocessing department must contribute.
There are different vigilance systems in operation in many regions. As an example, in the European Union, the medical device regulations place a legal responsibility on device manufacturers to report adverse incidents and Field Safety Corrective Actions (FSCAs) to EU Competent Authorities. Users of medical devices can also report incidents to the Competent Authority on their own jurisdiction. These reports contribute to a central database called EUDAMED. The US food and drug administration (FDA) operate a similar system and have their own database called the Manufacturer and User Facility Device Experience (MAUDE) database which contains all the medical device reports reported to the FDA since Aug 1996. Other countries such as Canada, Japan and Australia operate similar systems. Many of the regions now co-operate on regulation for medical devices via the International Medical Device Regulators Forum (IMDRF). |
Safe reprocessing is obtained by application of quality management principles by :
- RMD manufacturers: IFU’s include validated instructions for reprocessing. If needed, the maximum number of reuse is specified.
- Manufacturers of reprocessing equipment and consumables: Sterilizers, washer-disinfectors, cleaning and disinfecting agents, etc… comply to international standards and applicable regulation.
- Healthcare facilities: Detailed standard operating procedures (SOP’s) are defined for all reprocessing steps. All reprocessing chain links are key for patient safety: soils that are given time to dry on an RMD are more difficult to clean, an improperly cleaned RMD cannot be sterilized or disinfected, deficient packaging, transport, storage, or aseptic presentation may mean a contamination or damage of an RMD.
By process validation, a user verifies that:
- Installation of reprocessing equipment conforms to manufacturer’s recommendations
- IFU, test and calibration certificates are available.
- SOP’s are up to date. Il applicable, management of specific risk such as prion is included.
- Routine controls are in place.
- Training is executed. Training certificates are available.
- Occupational health and safety precautions are known and implemented.
- Medical devices vigilance obligations are known and enforced.
- Waste management measures are known and applied.
- Maintenance plans are in place for reprocessing equipment.
- Traceability is operational.

WFHSS recommendations for reprocessing of RMD's
- Persons in charge of reprocessing are consulted before purchase of a new RMD. It is verified that reprocessing methods recommended by RMD manufacturers are available to the health care facility. Specific attention is paid to complex RMD’s.
- Reprocessing Standard Operating Procedures (SOP’s) follow RMD IFU’s and applicable guidelines. If adaptations to an RMD manufacturer’s IFU are required they are to be justified, risk assessed and documented. When doubt exists between Spaulding categories, the highest available is chosen. If deficiencies are detected, they are reported according to applicable medical devices vigilance rules.
- RMD reprocessing is organized and implemented in partnership with care units and infection control. Implementation is clear from point of use to aseptic presentation. Prion risk, outbreaks and fragile patients are taken into consideration.
- Quality management and process validation are in place
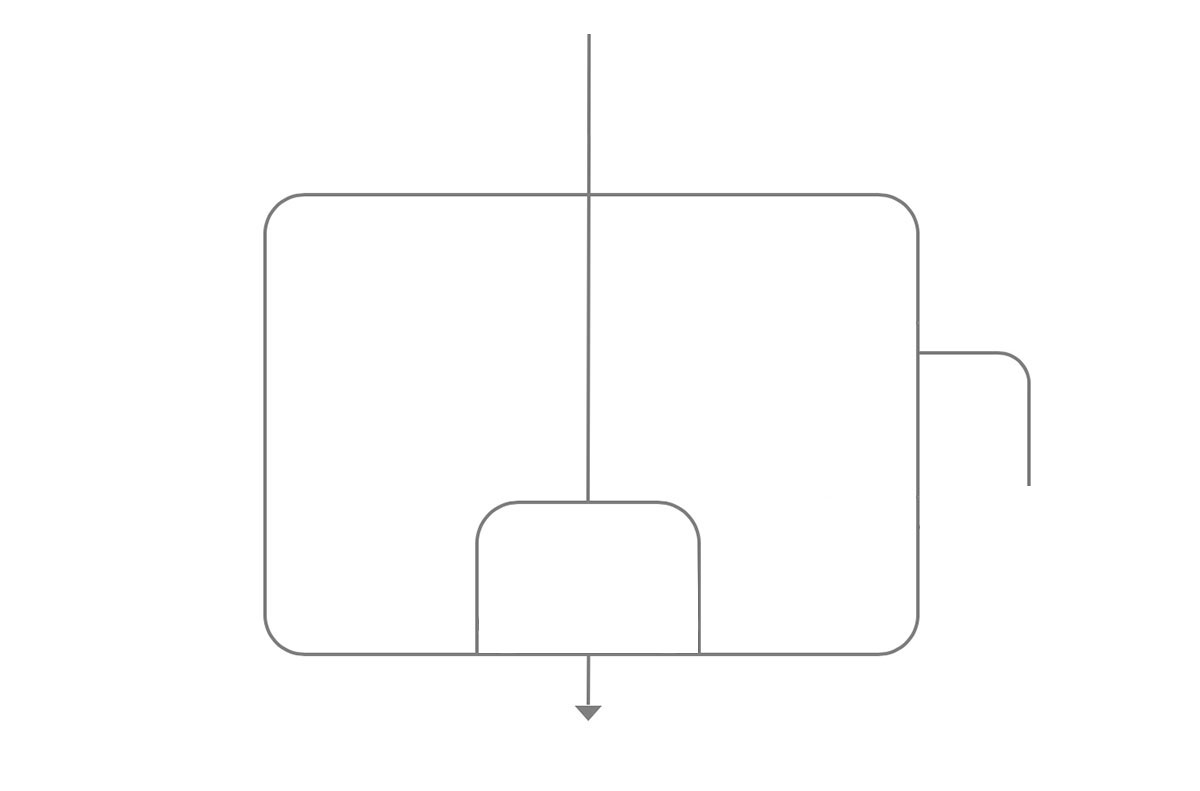
SOP’s according to Spaulding classification principles, Manufacturers IFU’s and applicable regulation
Go to ![]() Recommendations of WFHSS for reprocessing of RMD’s →
Recommendations of WFHSS for reprocessing of RMD’s →
contact with intact skin
Go to Spaulding classification principles →
2 of 13 Semi-criticalcontact with mucous or injured skin
Go to Spaulding classification principles →
3 of 13 CriticalContact with sterile tissue and vascular system
Go to Spaulding classification principles→
4 of 13 Evaluation of risk according to previous use (outbreak - prion)In partnership with care or surgical user and infection control
Go to ![]() Recommendations of WFHSS for reprocessing of RMD’s →
Recommendations of WFHSS for reprocessing of RMD’s →
Thorough cleaning and preparation of RMD
Go to ![]() recommendation of WFHSS for RMD →
recommendation of WFHSS for RMD →
Level of disinfection according to risk
Go to ![]() recommendation of WFHSS for RMD →
recommendation of WFHSS for RMD →
Sterilization method according to RMD manufacturer IFU and applicable regulation
Go to ![]() Recommendations of WFHSS for reprocessing of RMD’s →
Recommendations of WFHSS for reprocessing of RMD’s →
According to applicable regulation
Go to prion risk →
9 of 13 RMD safe for useFunctional, reprocessed according to manufacturer IFU’s and applicable regulation
Go to ![]() Recommendations of WFHSS for reprocessing of RMD’s →
Recommendations of WFHSS for reprocessing of RMD’s →
Consult services in charge of reprocessing before purchase of a new RDM
Go to![]() Recommendations of WFHSS for reprocessing of RMD’s →
Recommendations of WFHSS for reprocessing of RMD’s →
Validated processes
Go to ![]() recommendation of WFHSS for reprocessing of RMD’s →
recommendation of WFHSS for reprocessing of RMD’s →
Controls
Go to RMD and quality →
13 of 13- ISO 17664-1: Processing of health care products — Information to be provided by the medical device manufacturer for the processing of medical devices (2017)